This is a hard post to write, because it’s about the scariest aspect of diabetes care: hypoglycemia. HyPER glycemia is high blood sugar concentration, and a long-term risk for all people with diabetes. This post is about hyPO glycemia, very low blood sugar, and it’s a deadly situation.
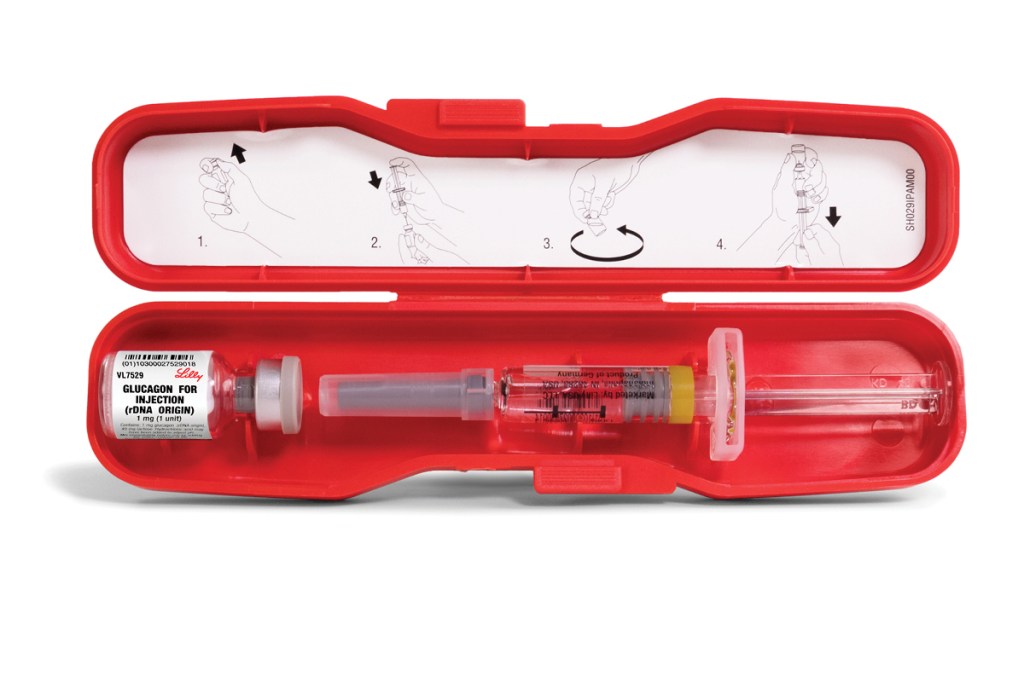
First of all, if your endocrinologist has somehow neglected to prescribe a glucagon syringe (pictured) get a prescription today (and maybe a new endo!).
Very low blood sugar deprives the nervous system of the chemicals it needs to function properly. The person suffering the “low” can lose consciousness and have seizures. If the low persists or worsens it can lead to death. Your perception of diabetes will change forever once your family experiences a hypo. Few things in life earn the term “terrifying.” A hypo with seizure is truly terrifying. It can be emotionally debilitating, because you now know that risk is always there, lying in wait. This is the part where I’m supposed to have something encouraging to say, but I got nuthin’. This sucks big time.
The main reason I write this post in a “beginning” diabetes blog, is because early after diagnosis, the person with diabetes will likely “feel” lows coming on, and may even be awakened. Sadly, crushingly, years of having blood sugar swings may make one less sensitive, and at risk of trending low overnight without recognizing it. For this reason, we consider Continuous Glucose Monitoring (CGM)to be a key component of the only humane health care course for those with diabetes. A CGM device with alarm, and preferably with “shutoff” control of insulin.
The glucagon pen above is the emergency treatment for someone who is low, likely recognized by entering siezure. I hate to break it to you, but a person with diabetes should never sleep alone. Good luck using that one at a singles bar! A sleepmate should always be in a position to recognize the twitching or thrashing of a seizure and trained to administer glucagon. The instructions are simple-enough, but you don’t want to be learning in the heat of an event! The glucagon triggers the liver to dump glucose into the blood stream, hopefully restoring consciousness.
To prevent low blood sugar events from reaching dangerous conditions, a CGM plus insulin pump work together to shut off insulin at selectable blood sugar concentrations. Modern pumps from Medtronic and Tandem can even use trending data to “Suspend Before Low” as the function is called. Living in great fear of hypos, we have selected the settings offering the highest-possible protection. Now, going without basal insulin for a while can result in a later “high,” but we’ve had good results in our household for the most part, with early morning blood sugars below 130 for the most part.
We’ll try to take up this dynamic interaction between automatic pumps and human metabolism at a later date. For the time being, get that glucagon and know where it is…and make sure you can hear, if not feel, your loved one who sleeps…and lives…with diabetes. Good luck! May these circumstances ever be strange to you and never experienced!
